Intellau_Celistic
5'3 KHHV Mentalcel
-
- Joined
- Aug 26, 2021
- Posts
- 166,462

A 44-year-old male firefighter initially presented with progressive lower back pain that appeared near the end of the day. He also noticed weakness in his right leg during stair-climbing and sit-to-stand transitions. He was otherwise healthy, a nonsmoker, and had no comorbidities.
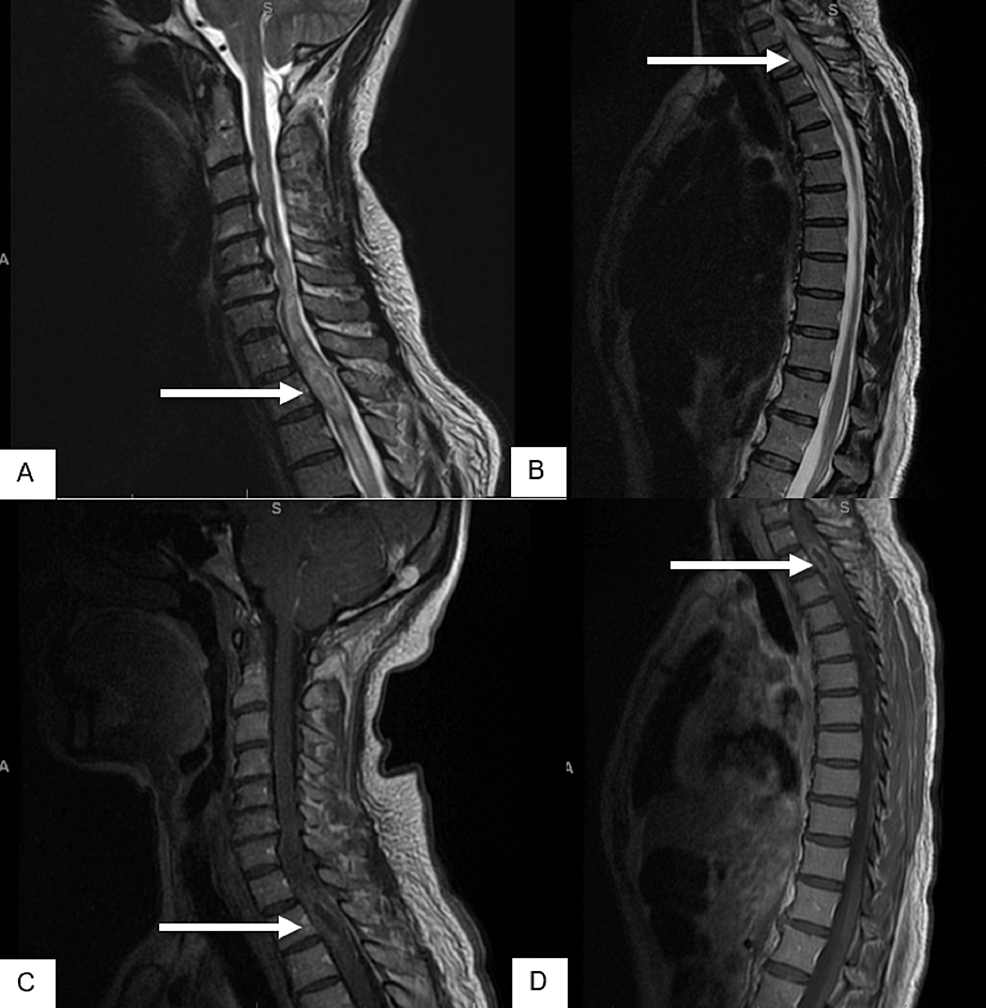
MRI of the lumbar spine demonstrated a non-enhancing intramedullary mass at the T11-12 level, which was T2-hyperintense and T1-isointense (Figure 3). Seven days after the onset of symptoms, he underwent microsurgical subtotal removal of the spinal cord tumor. Pathology review of the resected specimen established the diagnosis of primary spinal GBM, IDH-wild type, histone 3 mutation not reported. Computed tomography (CT) scan of the chest, abdomen, and pelvis was negative for distant metastases, while a follow-up MRI of the brain was also negative for intracranial disease. MRI of the entire spine done one-month post-operatively demonstrated residual enhancing intradural lesion at T11-T12 (Figure 4). The neurologic evaluation demonstrated a significant weakness in the right lower extremity. Sensory evaluation showed more impaired sensation on the right side compared to the left side.
Two months postoperatively, he developed progressive symptoms, and a follow-up MRI demonstrated residual enhancing mildly heterogeneous solid mass at the T11-12 level measuring 4 cm in length and 1.2 cm in greatest diameter. After a thorough discussion, the patient decided to undergo gross total resection of the intramedullary spinal cord tumor to try to extend his life regardless of the deficits he would incur with radical resection. Sixty-three days after the onset of symptoms, the patient underwent gross total resection of the residual spinal cord tumor. Following surgery, the patient had no strength in his lower extremities and no sensation below the level of the umbilicus. He used a Foley catheter and had fecal incontinence. The pathology from the initial biopsy was reviewed at the Mayo Clinic and confirmed to be primary spinal GBM.
His case was discussed at a multidisciplinary neuro-oncology conference where an imaging review noted some suspicion of possible residual disease in the lower end of the resection area, with a higher potential for residual disease inferior to the gross tumor (Figure 5). After discussion, the group decided to proceed with adjuvant radiation therapy. Three and a half months after initial resection, the patient received adjuvant radiation therapy to a total dose of 59.4 Gy in 33 fractions using the VMAT technique, including the volume 5 cm above and below the original lesion (Figure 6). The absence of function to preserve allowed the use of full-dose radiation therapy. The planning aim was to cover at least 95% of the PTV with 98% of the prescribed dose. The dose constraint for both kidneys was a mean dose < 15 Gy, the small bowel was V45 < 195 cc and the liver was a mean dose < 30 Gy. The role of systemic chemotherapy, specifically with temozolomide, was uncertain because of the rare presentation of GBM in the spinal cord and the lack of documented evidence of efficacy. However, considering the patient’s young age, tumor location, absence of comorbidities, and extreme motivation to seek treatment, chemotherapy was recommended with temozolomide 75 mg/m2 daily concurrent with radiation treatment.
The patient experienced mild to moderate nausea and vomiting during the first few weeks of his radiation therapy, which were managed with anti-emetics. He was hospitalized throughout his treatment to undergo physical rehabilitation. There was no significant dermatitis, pain, or diarrhea.
Four weeks post-radiation therapy, he started the first of a planned six cycles of adjuvant temozolomide, 150 mg/m2, for five days every 28 days. At six weeks post-radiation therapy, he still experienced persistent nausea. Follow-up MRI scans were pending; however, the patient had a seizure in the interim. A cranial CT scan revealed two enhancing soft tissue masses within the anterior horn of the left lateral ventricle (1.6 cm x 2.4 cm x 2.5 cm) and at the base of the fourth ventricle (2.6 cm x 2 cm x 1.7 cm) with hydrocephalus and diffuse dural enhancement suggestive of intracranial disease progression (Figure 7). A small focus of high density was noted within the tumor involving the fourth ventricle suggestive of a small bleed. Further investigations were not performed, as the patient’s condition deteriorated quickly, and he expired three days after the seizure, 7.4 months after the pathologic diagnosis.
Two Cases of Primary Spinal Glioblastoma in Adults Treated With Multimodality Therapy
Primary spinal glioblastoma (GBM) is a rare disease entity with no established standard treatment. We present two cases of primary spinal GBM initially presenting with motor-sensory deficits and back pain. Management varied in that the first patient received subtotal resection followed by...www.cureus.com